|
Clinical Image
Purtscher-like retinopathy secondary to dermatomyositis
1 PGY3 Resident, Department of Ophthalmology, University of Texas Health at San Antonio, San Antonio, Texas, United States
2 Retina Fellow, Department of Ophthalmology, University of Texas Health at San Antonio, San Antonio, Texas, United States
Address correspondence to:
Logan Russ Vincent
MD, UT Health San Antonio Medicine, 7703 Floyd Curl Dr. MSC 6230, San Antonio, Texas 78229-3900,
United States
Message to Corresponding Author
Article ID: 100009Z17LV2019
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Vincent LR, Beck L. Purtscher-like retinopathy secondary to dermatomyositis. J Case Rep Images Opthalmol 2019;2:100009Z17LV2019.ABSTRACT
No Abstract
Keywords: Dermatomyositis, Purtscher-like retinopathy, Retina
Case Report
A 18-year-old Caucasian male with no previous past medial history presented with two weeks of progressively worsening blurry vision, proximal muscle weakness, myalgia, ataxia, rash on knuckles and back, dark colored urine, and dysphagia. The patient denied any ocular history, medication use, or illicit drug use. He was now bed bound and unable to move his arms or legs independently. The patient recently completed high school and denied any recent travel, change in diet, sick contacts, or family history of rheumatologic disorders.
On admission, the patient had creatinine kinase of 29,006 U/L, elevated liver enzymes, thrombocytopenia, and elevated CRP with subsequent diagnosis of rhabdomyolysis. On physical examination, he exhibited a shawl sign and Gottron’s papules. The patient also had a quadriceps muscle biopsy performed which showed nonspecific myopathic changes, but results were confounded since the patient was initiated on steroid therapy prior to biopsy. The patient was diagnosed with dermatomyositis with the above mentioned clinical findings.
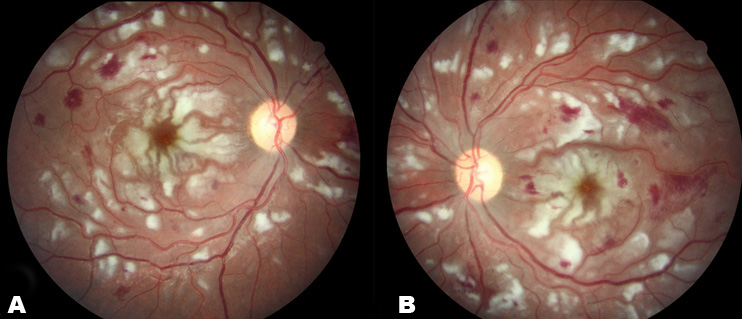
On ocular examination, vision measured 20/250 in the right eye and 20/300 in the left eye at distance. There was no acute pathology on anterior segment examination. Dilated fundus examination showed numerous cotton wool spots, retinal hemorrhages, and Purtscherflecken confined to the posterior pole (Figure 1). These findings prompted the diagnosis of Purtscher-like retinopathy. The patient was discharged to an outpatient rehab facility on oral prednisone and treated with infusions of rituximab monitored by Rheumatology. At two week follow up, the patient’s vision was 20/40 and 20/300 at distance and white retinal lesions had decreased in number and size. The patient was receiving daily physical therapy which allowed him to transfer independently and ambulate longer distances with a walker.
Discussion
Purtscher retinopathy, first described by Otmar Purtscher in 1910 in a patient with cranial trauma, clinically presents as a chorioretinopathy with retinal findings including cotton-wool spots, retinal hemorrhages, optic disc edema, and areas of inner retinal whitening (Purtscher-flecken) [1],[2]. Miguel et al., published updated diagnostic criteria for Purtscher retinopathy which requires 3 out of 5 of the following: Purtscherflecken, retinal hemorrhages in low to moderate number, cotton-wool spots confined to posterior pole, probable explanatory etiology (e.g. trauma, chest compressions, etc.), and complementary investigation compatible with diagnosis. By definition, Purtscher-like retinopathy occurs without a history of trauma and etiologies include acute pancreatitis, chronic renal failure, connective tissue disorders such as lupus, scleroderma, dermatomyositis, and preeclampsia [1]. There are no evidence-based guidelines on treatment, and therapy is focused on treating the underlying etiology. High-dose, intravenous steroids remain a commonly initial treatment regimen, but the efficacy of steroids has not been established in prospective trails and remains controversial [1],[3].
Retinopathy associated with dermatomyositis is an uncommon entity first described by Bruce in 1938 [4]. Retinopathy associated with dermatomyositis is rare and has only been described in a few case reports in the literature. Yan et al. described an 18-year-old Chinese female diagnosed with Purtscher-like retinopathy associated with dermatomyosistis that presented with decreased vision and lower extremity weakness that was subsequently treated with systemic corticosteroid [5]. Bader-Meunier et al. reported a 7-year-old with juvenile dermatomyositis and thrombotic thromobocytopenic purpura treated with emergent plasmaphoresis, which resulted in the improvement of the retinopathy [6]. Barreiro-Gonzalez et al. described an 11 year-old female with dermatomyositis diagnosed with Purtscher-like retinopathy after cotton wool spots, flame hemorrhages, and venous tortuosity were found on dilated fundus examination [7]. In patients with dermatomyositis, the retinopathy usually resolves without vision loss, but permanent vision loss can occur from severe macular hemorrhage and optic atrophy [8].
Conclusion
Purtscher-like retinopathy is an uncommon retinal pathology that is associated with multiple systemic diseases. While systemic steroids are commonly used in initial treatment, therapy should be focused on treating the underlying cause of the retinopathy. The association with dermatomyositis is rare and has only been described in few case reports in the literature.
REFERENCES
1.
Miguel AI, Henriques F, Azevedo LF, Loureiro AJ, Maberley DA. Systematic review of Purtscher’s and Purtscher-like retinopathies. Eye (Lond) 2013;27(1):1–13. [CrossRef]
[Pubmed]

2.
3.
Agrawal A, McKibbin M. Purtscher's retinopathy: Epidemiology, clinical features and outcome. Br J Ophthalmol 2007;91(11):1456–9. [CrossRef]
[Pubmed]

4.
Bruce GM. Retinitis in dermatomyositis. Trans Am Ophthalmol Soc 1938;36:282–97.
[Pubmed]

5.
Yan Y, Shen X. Purtscher-like retinopathy associated with dermatomyositis. BMC Ophthalmol 2013;13:36. [CrossRef]
[Pubmed]

6.
Bader-Meunier B, Monnet D, Barnerias C, et al. Thrombotic microangiopathy and Purtscher-like retinopathy as a rare presentation of juvenile dermatomyositis. Pediatrics 2012;129(3):e821–4. [CrossRef]
[Pubmed]

7.
Barreiro-González A, Cerdà-Ibáñez M, Barranco González H, et al. Purtscher-like retinopathy associated with dermatomyositits and hemophagocytic lymphohistiocytosis. [Article in Spanish]. Arch Soc Esp Oftalmol 2018;93(4):202–5. [CrossRef]
[Pubmed]

8.
Backhouse O, Griffiths B, Henderson T, Emery P. Ophthalmic manifestations of dermatomyositis. Am Rheum Dis 1998;57(8):447–9.
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Logan Russ Vincent - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Kinley Beck - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2019 Logan Russ Vincent et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.