|
Case Report
Posterior dislocation and early retrieval of a Descemet stripping automated endothelial keratoplasty graft
1 Khoo Teck Puat Hospital, Singapore
Address correspondence to:
Philip Francis Stanley
Khoo Teck Puat Hospital,
Singapore
Message to Corresponding Author
Article ID: 100048Z17PS2025
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Stanley PF, Hang YT, Jue JC. Posterior dislocation and early retrieval of a Descemet stripping automated endothelial keratoplasty graft. J Case Rep Images Opthalmol 2025;8(2):12–18.ABSTRACT
Introduction: This case report seeks to document a rare case of posterior dislocation of Descemet stripping automated endothelial keratoplasty (DSAEK) graft in a patient with subluxed intraocular lens one day post-operation.
Case Report: A 70-year-old man with a background of subluxed intraocular lens in a non-vitrectomized eye with pseudophakic bullous keratopathy underwent DSAEK. Review on post-operative day one noted a dislocated graft. Graft re-bubbling in the clinic with air displaced the graft into the posterior segment. Graft retrieval, repositioning, and intraocular lens removal were done on the same evening without complications.
Conclusion: This case report shows the possibility of DSAEK graft dislocation post-operation in a non-vitrectomized eye but with compromised barrier between anterior and posterior chambers of the eye. The uniqueness of this case report is retrieving a DSAEK graft in the posterior segment and successfully using the same graft to achieve a clear cornea the day after the original surgery.
Keywords: Descemet stripping automatic endothelial keratoplasty, Graft dislocation, Posterior, Subluxed intraocular lens
Introduction
Descemet stripping automated endothelial keratoplasty (DSAEK) is a partial corneal transplant which replaces only the posterior corneal tissue compared to penetrating keratoplasty (PK), which are full thickness corneal transplants. It is suggested to have faster visual rehabilitation and a lower risk of complications compared to PK [1].
Posterior graft dislocation is a known [2] post-operative complication of DSAEK, with possible predisposing risk factors such as previous vitrectomy, aphakia, or complicated intraocular lens placement [3].
We present a case of a 70-year-old gentleman with a background of subluxed intraocular lens but non vitrectomized eye with pseudophakic bullous keratopathy who underwent DSAEK and subsequently had a posteriorly dislocated graft.
Case Report
A 70-year-old Chinese male presented to Eye Clinic in November 2023 with blurring of vision with pain in left eye for one week. The patient has a known past ocular history of subluxed intraocular lens in the left eye which underwent cataract operation in 2012. There is no history of prior vitrectomy. On presentation, visual acuity of right eye is 6/7.5+2 while left eye was counting fingers closely. Intraocular pressure was 14 mmHg on the right and 10 mmHg on the left.
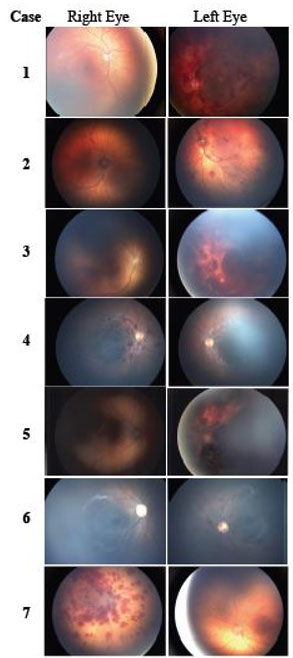
On examination of the left eye, there noted to be bullous keratopathy with microcystic edema and severe Descemet membrane folds. Endothelial cell count by specular microscopy was 2506/mm2 in the right eye and 749/mm2 in the left eye (Figure 1). The anterior chamber was deep with occasional cells but no vitreous. The intraocular lens was subluxed but still in the iris plane. The decision to address the pseudophakic bullous keratopathy instead of addressing the mild lens dislocation first was made because there was significant corneal oedema impeding the view of the anterior chamber and intraocular lens. A clear view and repeat intraocular lens calculations after the DSAEK graft was the thought process. Examination of the right eye was normal.
The patient underwent DSAEK of the left eye in March 2024. The donor tissue was obtained from Eversight, Chicago, Illinois with a death to preservation time of 11 hours and 48 minutes. Endothelial cell density was 2915 cells/mm2. Locally, the Singapore Eye Bank prepared the tissue. Pre- and post-microkeratome cut endothelial cell density was 3030 cells/mm2 and the graft thickness was 107 microns as measured by anterior segment optical coherence tomography (OCT). Intra-operatively, the donor was cut to 8.0 mm. Graft insertion was done using the Tan ultrathin Endoglide. Anterior vitrectomy was necessary since vitreous was seen in the anterior chamber coming around the dislocated intraocular lens (IOL). A 70% of air bubble provided good graft attachment.
On review the day after operation, it was noted that the graft has separated with no air bubble seen (Figure 2). The previously subluxed IOL was now dislocated. Management options were an air bubble injection through a side port in the clinic versus a SF6 re-bubble that would require scheduling in the day surgery operating theatre. The clinic procedure was chosen as a quicker and cheaper solution. Unfortunately, the DSAEK graft edge was adjacent to the side port, and the 27-gauge needle touched the graft, and the air inserted itself between the graft and the host cornea. The graft was displaced into the posterior segment of the eye.
The patient was immediately consented for pars plana vitrectomy (PPV) with intraocular lens (IOL) removal and DSAEK graft removal and repositioning the same evening as an emergency add on case. During the PPV procedure the mildly dislocated IOL became vertically orientated and it was grasped with micro forceps and brought though the pupil and out the original DSAEK surgery corneal wound. The decision was made to leave the patient aphakic since a secondary IOL procedure would have added considerable time to the procedure and may have compromised the DSAEK graft that needed the SF6 bubble for attachment.
The posteriorly dislocated graft was retrieved through a pars plans vitrectomy and reused by repositioning it in the anterior chamber. The concave orientation of the DESAK graft was identified during the vitrectomy and grasped with micro-forceps, pulled through the pupil and positioned in the anterior chamber while a sulfur hexafluoride (SF6) bubble was injected quickly. The graft was noted to be in the correct orientation.
The patient was given post-operative instructions to lie strictly supine for 1 hour and then supine as much as possible on the ward overnight to allow optimal positioning of the SF6 bubble. The patient was then reviewed in clinic the next day and started on Vigamox and Pred Forte eyedrops every 3 hourly to the left eye. Post-operative day one anterior segment OCT showed full graft attachment (Figure 3).
The patient was then reviewed again three days later, and the graft was well attached with no gas bubble. The patient was then reviewed again in 1 week, 4 weeks, 6 weeks, and 3 months post-operation, and the graft remained well attached after the SF6 bubble dissipated (Figure 4). Repeated endothelial cell count about one month post-graft retrieval and re-attachment in April of 2024 noted an increase of the cell counts to 1006/mm2 in the left eye (Figure 5). Vigamox eyedrops were stopped at one month post-operation. Pred Forte eyedrops were tapered to 4 times a day for a month, 3 times a day for a month and kept at 2 times a day at three months post-operation.
Once the DSAEK graft provided a clear cornea and the aphakic refraction was stable, the secondary IOL procedure was carried out. This was five months postoperation, and the patient was counselled and listed for vitrectomy and secondary IOL. The patient was then seen at one day, one week, two weeks, one month, and two months post-operation, and the graft was clear at each visit. On 16 October 2024 two months post-operation, the patient’s visual acuity was 6/12+1 in the left eye, and with refraction improved to 6/7.5+2.
The patient was kept on regular follow up since then. Figure 6 shows the latest anterior segment OCT. Figure 7 shows the most recent endothelial cell density of 2198/mm2. Figure 8 shows a slit lamp photograph showing a clear cornea and a well centered IOL, all done on 25 February 2025.
The patient’s consent for his case report to be used in research writing was obtained during one of his regular clinic reviews post-operatively.
Discussion
Graft dislocation is the most frequently reported complication after DSAEK due to potential causes such as interface fluid or air, minimal traction provided by smooth recipient interface for donor graft or patient squeezing or eye rubbing [1],[4].
However, in patients with an insufficient barrier between the anterior and posterior chambers of the eye such as defects in the iris or lens capsule, there may be further possibility of posterior dislocation of DSAEK grafts into the vitreous cavity either intra-operatively or post-operatively.
A literature review was done by looking at case reports on posterior dislocation of DSAEK grafts on PubMed with the findings summarized in Table 1.
One of the strongest proposed risk factors for posterior dislocation of DASEK graft is the presence of a decompartmentalized eye affecting graft apposition. The proposed mechanism is that in a decompartmentalized eye, there is a loss of the closed system inside the anterior chamber with little turbulence. Fluid infusion via anterior chamber maintainer would lead to increased turbulence which causes the DSAEK graft to move from its intended position before the air bubble could be injected [5],[6]. Air movement into the vitreous cavity could prevent sufficient maintenance of tamponade effect [7]. In our presenting case study, patient was noted to have a subluxed IOL with vitreous noted in the anterior chamber coming around the subluxed IOL, which suggested a breach in the closed system of the anterior chamber. Furthermore, the air bubble was noted to be approximately 70% post-operatively but on post-operative day one review, the previously subluxed IOL was dislocated and there was no air bubble seen, suggesting the likely migration of the air bubble into the vitreous cavity after the complete dislocation of the IOL, thus affecting the tamponade effect on the graft and causing graft dislocation. Further attempts to re-bubble the graft caused the graft to migrate posteriorly into the vitreous cavity due to the open communication between anterior and posterior segment from the dislocated IOL.
To reduce the risk of graft dislocation in high-risk patients, putting temporary trans-corneal fixation sutures as part of the primary DSAEK procedure is a promising outlook with little complication and good graft adherence post-operation [8]. Even in graft dislocation, placement of full thickness sutures over the detached area can help with good apposition [9].
When posterior graft dislocation arises, the timing for graft retrieval is crucial as there is a correlation between the time taken for graft retrieval and posterior segment complications such as cystoid macular edema or retinal detachment. In general, cases with graft retrieval at time of dislocation or within few days later were associated with no posterior segment complications while those with graft retrieval weeks after dislocation was associated with tractional retinal detachment. There are proposed mechanisms in how posterior dislocated graft can cause retinal detachment. Firstly, a histopathological study of failed DSAEK grafts noted pathological findings of fibrocellular tissue proliferation and epithelial ingrowth, which may predispose to graft adherence to retinal surface. The presence of transplanted foreign ocular tissue in vitreous cavity may evoke a severe inflammatory response which predisposes to early proliferative vitreoretinopathy. Hence, delayed removal of dislocated graft could result in further complications like retinal detachment [10]. Hence in our case study, when the graft was noted to be dislocated, an emergency operation was arranged the same evening to ensure the least amount of delay between the dislocation of the graft and the retrieval. This short time frame between dislocation of graft and retrieval could contribute to the reason why the patient did not develop any posterior segment complications such as tractional retinal detachment. This was documented by other case studies in our literature review which had a prolonged wait of a few weeks between graft dislocation and retrieval. The good visual acuity the patient achieved after secondary IOL implantation (6/7.5+2) may also be due to the timely retrieval of the dislocated graft. Our literature review suggests that a delay in graft retrieval time could be correlated with a poorer visual outcome.
We have presented a case study of an uncommon case of which a posterior dislocation of graft has occurred due the decompartmentalization of the eye following a dislocated IOL. Further research into this area can help to improve on current techniques of DSAEK to tailor towards patients at higher risk of posterior graft detachment as well as targeted management to reduce complications if detachment happens.
Conclusion
This case report shows the increased risk of DSAEK graft dislocation post-operation in a non-vitrectomized eye with a compromised barrier between anterior and posterior chambers of the eye. Pre-operatively, if the patient is known to be at high risk for a DSAEK graft dislocation, temporary trans-corneal fixation sutures can be considered as part of the primary DSAEK procedure and/or to use sulfur hexafluoride (SF6) gas instead of air. If the graft still dislocates posteriorly, an early operation to retrieve the graft may reduce the chance of posterior segment complications. This case report also highlights successfully using the same retrieved dislocated graft to achieve a good clinical outcome and can be applied to similar cases in future.
REFERENCES
1.
Kim SE, Lim SA, Byun YS, Joo CK. Comparison of long-term clinical outcomes between Descemet’s stripping automated endothelial keratoplasty and penetrating keratoplasty in patients with bullous keratopathy. Korean J Ophthalmol 2016;30(6):443–50. [CrossRef]
[Pubmed]

2.
Suh LH, Yoo SH, Deobhakta A, Donaldson KE, Alfonso EC, Culbertson WW, et al. Complications of Descemet’s stripping with automated endothelial keratoplasty: Survey of 118 eyes at One Institute. Ophthalmology 2008;115(9):1517–24. [CrossRef]
[Pubmed]

3.
Afshari NA, Gorovoy MS, Yoo SH, Kim T, Carlson AN, Rosenwasser GOD, et al. Dislocation of the donor graft to the posterior segment in Descemet stripping automated endothelial keratoplasty. Am J Ophthalmol 2012;153(4):638–42, 642.e1–2. [CrossRef]
[Pubmed]

4.
Price MO, Price FW. Descemet’s stripping endothelial keratoplasty. Curr Opin Ophthalmol 2007;18(4):290–4. [CrossRef]
[Pubmed]

5.
Sng CCA, Mehta J, Tan DT. Posterior dislocation and immediate retrieval of a Descemet stripping automated endothelial keratoplasty graft. Cornea 2012;31(4):450–3. [CrossRef]
[Pubmed]

6.
Grueterich M, Messmer E, Kampik A. Posterior lamellar disc dislocation into the vitreous cavity during Descemet stripping automated endothelial keratoplasty. Cornea 2009;28(1):93–6. [CrossRef]
[Pubmed]

7.
Tanaka H, Hirano K, Horiguchi M. Wheel spokes technique for endothelial keratoplasty for extremely mydriatic bullous keratopathy eyes without capsular support. Case Rep Ophthalmol 2018;9(1):238–42. [CrossRef]
[Pubmed]

8.
Papathanassiou M, Papaioannou L. Suturing technique to promote graft attachment in challenging cases of Descemet stripping endothelial keratoplasty. Open Journal of Ophthalmology 2015;5(3):124–9. [CrossRef]

9.
Wu WK, Wong VWY, Chi SCC. Graft suturing for lenticule dislocation after Descemet stripping automated endothelial keratoplasty. J Ophthalmic Vis Res 2011;6(2):131–5.
[Pubmed]

10.
Singh A, Gupta A, Stewart JM. Posterior dislocation of Descemet stripping automated endothelial keratoplasty graft can lead to retinal detachment. Cornea 2010;29(11):1284–6. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Philip Francis Stanley - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Yeo Tun Hang - Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Jenny Chen Jue - Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2025 Philip Francis Stanley et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.