|
Case Report
A rare case of pediatric teen orbital alveolar subtype rhabdomyosarcoma in Saudi Arabia Eastern Province: A case report
1 Department of Ophthalmology, King Fahad Hospital of the University, Imam Abdulrahman Bin Faisal University, Khobar, Saudi Arabia
2 Department of Ophthalmology, Dhahran Eye Specialist Hospital, Dhahran, Saudi Arabia
3 Department of Ophthalmology, King Fahd Military Hospital, Dhahran, Saudi Arabia
4 Ophthalmology Department, College of Medicine, Shaqra University, Riyadh, Saudi Arabia
5 Oculoplastic Division, Department of Ophthalmology, King Fahad Hospital of the University, Imam Abdulrahman Bin Faisal University, Khobar, Saudi Arabia
Address correspondence to:
Raghad Mohammad Alakel
Department of Ophthalmology, King Fahad Hospital of the university, Imam Abdulrahman Bin Faisal University, Khobar,
Saudi Arabia
Message to Corresponding Author
Article ID: 100047Z17RA2025
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Alakel R, Algarni S, Alharbi A, Alhadlag A, Nassim H. A rare case of pediatric teen orbital alveolar subtype rhabdomyosarcoma in Saudi Arabia Eastern Province: A case report. J Case Rep Images Opthalmol 2025;8(2):5–11.ABSTRACT
Introduction: To report a rare presentation of an alveolar orbital rhabdomyosarcoma and the corresponding findings on computed tomography (CT), magnetic resonance imaging (MRI), and surgical outcome.
Case Report: A 14-year-old Saudi boy, who presented with a progressively enlarging left upper eyelid mass. Associated with proptosis and limitation of extra-ocular muscles. He underwent imaging including CT scan and MRI which both modalities showed a large left intraconal mass with extraconal extension. The patient underwent a subtotal excision of the mass. Biopsy was sent for histopathology revealed a diagnosis of alveolar rhabdomyosarcoma, solid variant. Histogenetics, including fluorescence in situ hybridization (FISH) analysis for the FOXO1 gene, showed a negative gene rearrangement. The patient was referred to the oncology center in Dammam for confirmation of the diagnosis and to initiate appropriate management based on the disease stage.
Conclusion: This case report highlights a rare instance of orbital alveolar rhabdomyosarcoma (RMS) in a 14-year-old boy from the Eastern Province of Saudi Arabia. Despite being a highly malignant tumor with aggressive progression typically affecting younger children, our patient presented with a relatively slower progression and a 6-week history of enlarging swelling and non-axial proptosis.
Keywords: Alveolar subtype, Orbital rhabdomyosarcoma, Pediatric oncology
Introduction
Rhabdomyosarcoma (RMS) is a rare, aggressive, and lethal mesenchymal-originated tumor [1]. It is the most frequent pediatric head and neck soft tissue sarcoma, with 10% of cases developing in the orbit [1]. It is predominantly a childhood disease with young children of 5–7 years being affected on average [2]. However, it can present between birth and the age of seven, with more than 90% of cases occurring before the age of 16 years [1],[2]. Several studies have reported a male preponderance; however, many series have observed no sex or racial predilection [3],[4]. It may sometimes follow a traumatic event [5]. Histologically, RMS can be classified into four main types: pleomorphic, embryonal, alveolar, and spindle cell/sclerosing. The embryonal type is the most prevalent, while the pleomorphic subtype is nearly exclusive in adult patients, and the alveolar subtypes are very rare. The PAX3/7-FOXO1 gene is present in the majority of alveolar cases and is associated with the poorest prognosis [6],[7],[8],[9],[10].
The primary site of orbital rhabdomyosarcoma is often within the superior portion of the orbit [11] in a paper by Bastola et al. They reported that proptosis was the most typical presenting symptom, being present in every reviewed case [7]. Rhabdomyosarcoma generally manifests with unilateral non-axial proptosis, ptosis, and eyelid swelling [12]. Other conditions include orbital disease and neoplasms that may resemble those of RMS. Some of these entities will also be considered with a detailed history and clinical examination like orbital cellulitis, lymphangioma, optic nerve glioma, optic nerve meningioma and Langerhans cell histiocytosis/Langerhans granulomatosis, hemangioma, and dermoid cyst [13]. The disease can mimic infections or inflammations in that the disease process is sometimes characterized by an acute onset and rapid development [14]. Imaging examination, such as MRI and CT, is necessary to make an accurate diagnosis for the lesion, preoperative determination of the size, shape and location of tumor or settlement line sign or bone destruction. Imaging is also necessary to monitor the patient for residual or recurrent lesions. In the first three years, relapses typically occur. The most common site of metastasis is the lung [13].
Treatment options are radical or partial surgical resection, chemotherapy, external beam radiotherapy (EBRT), brachytherapy, and exenteration as the last resort [15]. As histopathologic confirmation is required for diagnosis of rhabdomyosarcoma, biopsy before treatment is mandatory. However, the literature is inconclusive in terms of whether incisional or excisional biopsy should be favored [16]. Some experts believe that no more than an incisional biopsy should be performed to verify the initial diagnosis because both chemotherapy and radiation therapy have improved [1]. But others say that chemotherapy and radiation therapy are more effective when as much tumor tissue as possible is removed. The sooner diagnosis and treatment are made, the better the results and prognosis.
The objective of this case report is to contribute to the current literature and record an unusual case of orbital RMS. It achieves this through clinical signs, the difficulties in diagnosis, and treatment outcomes, to help simplify this rare cancer so that it may be better understood. Moreover, to the best of our knowledge, there are no similar published cases in the Arabic Gulf area yet that emphasize the novelty and clinical importance of our report. Recording this unusual case helps to enrich the literature locally, and it offers some impact to clinicians who will handle cases with such a presentation in the future.
Case Report
A 14-year-old boy, previously healthy and without known allergies, arrived at the Emergency Room (ER) at King Fahad University Hospital in Khobar, Saudi Arabia. He said he had a lump on his left upper eyelid that had been there for a month. His mother said that the mass started out as a small localized lesion and then got bigger over time.
The patient was quickly sent from the ER to the on-call ophthalmology team. The results of a full eye exam are as follows: Visual acuity (Vasc): The right eye (OD) has 20/20 vision, and the left eye (OS) has 20/30 vision. Goldmann measured the intraocular pressure (IOP). The right eye (OD) had a pressure of 17 mmHg, and the left eye (OS) had a pressure of 24 mmHg, according to applanation tonometry.
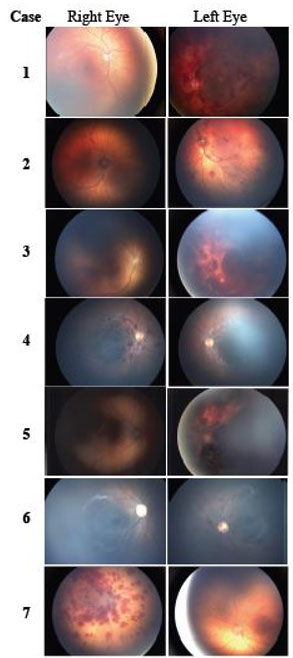
Pupils: Round, regular, and reactive to light with no afferent pupillary defect (APD) in both eyes (OU). Color vision: 13/13 for both eyes (OU). Extra-ocular muscle showed: Limitation on supraduction OS. Slit Lamp Examination: Lids/Lashes: Within normal limits for the right eye (OD), with a large palpable mass approximately 3 cm in size creating dystopia, rubbery in nature in the left eye (Figure 1). Remaining of his slit lamp examination including his dilated fundus exam were unremarkable (Figure 1).
Given these findings, the patient was referred to the oculoplastic division for further evaluation. An orbital CT scan with contrast and MRI were requested.
The CT scan showed a lobulated mass with a density between low and medium in the superomedial anterior left orbit. The mass was 2.8 cm wide, 2.9 cm long, and 1.7 cm high in mediolateral, anteroposterior, and craniocaudal directions. It showed avid heterogeneous enhancement, which pushed the left globe down and changed its shape, and the left superior vein was slightly engorged. The mass did not extend into the brain and did not touch the orbital apex. Bone remodeling was observed in the superior region of the left orbit. These findings were suggestive of a longstanding lesion, likely an orbital vascular or lymphatic malformation (Figure 2). Computed tomography chest showed no signs of metastasis to lung nodules. Positron emission tomography (PET) scan did not show any bony or nodal suspicious nodal disease.
The intravenous (IV) contrast orbital MRI showed a large mass in the left intraconal space that went outside of it. The mass looked mostly dark on T1-weighted imaging (T1WI) and bright on T2-weighted imaging (T2WI). It also had a lot of empty spaces inside that were filled with blood vessels. After the contrast, the images showed a lot of improvement, mostly at the edges. The lesion was inseparable from the lateral rectus muscle, which also showed enhancement. The superior rectus and superior oblique muscles were compressed inferiorly. A smaller, likely connected lesion was noted medially with similar features, causing a mass effect on the globe without direct invasion. The left lacrimal gland was displaced inferolaterally. The mass measured 3.6 × 2.6 × 2.2 cm in anteroposterior (AP), transverse (TR), and craniocaudal (CC) dimensions. Bone remodeling without destruction was observed. There was no evidence of effusion restriction. The right orbit, extraocular muscles, lacrimal gland, and retrobulbar orbital fat were unremarkable. No intra- or extraconal lesions were seen. These findings were consistent with a cavernous hemangioma (Figure 3).
As a result, the patient was scheduled for surgery to remove the mass. The lab work and anesthesia clearance that needed to be done before the surgery were done. The patient was ready for surgery and covered with a blanket while under general anesthesia. The crease in the upper eyelid was marked, and local anesthesia was given. A sharp dissection was performed with a blade, and a blunt dissection above the tumor. The two lobes of the tumor (attached to the superior oblique muscle and trochlea) were completely resected (Figure 4) and measured at 4.5 cm by 2.5 cm in size (Figure 5). The patient received a gentamycin wash, and an incision was left open with a glove finger drain after excision. The incision was closed medially with 4-0 silk sutures and the lid crease with four 5-0 Vicryl sutures and an extra 7-0 Vicryl suture. Tobramycin/dexamethasone ointment was applied. The patient was extubated on the operating table, and a histopathological examination of the tumor was requested for diagnosis.
After the surgery, the patient stayed in the hospital for two days with the bed tilted at a 45° angle. Post-operative care involved the application of an ice pack for 15 minutes, repeated every hour, and the administration of tobramycin/dexamethasone ointment within the eye and on the eyelid twice daily. Additionally, the patient was given oral prednisolone 30 mg once daily, oral amoxicillin-clavulanic acid 1 g twice daily, and pantoprazole 20 mg once daily. Four hours post-operation, the patient was examined. Visual acuity was 20/20 OD and 20/50 OS, and the pupils were round, regular, and reactive to light with no afferent pupillary defect. The anterior segment examination revealed the left upper and lower lids were edematous, erythematous, and non-tender, with sutures and a finger drain in place. There was subconjunctival hemorrhage and congested conjunctiva.
Upon discharge, the finger drain was removed. The patient received a prescription for oral Amoxicillin/Clavulanic acid 1 g twice a day for 10 days, fusidic acid ophthalmic ointment twice a day for 7 days, paracetamol 500 mg orally every 6 hours for 5 days, and lubricating drops.
After a week, the histopathology results showed that the patient had alveolar rhabdomyosarcoma, solid variant. The gross description said that there were two pieces of gray-tan soft-firm tissue that were not oriented. The smallest piece was 1 × 0.9 × 0.5 cm and the largest was 4.5 × 2.5 × 1.9 cm. The outer surface was inked black, and serial sections showed a white-gray rubbery fleshy cut surface with no necrosis or hemorrhage. The specimen was entirely submitted in eight cassettes. Microscopic examination: (Figure 6).
The histogenetics, including fluorescence in situ hybridization (FISH) analysis for the FOXO1 gene, showed a negative gene rearrangement. This result is was also confirmed in another lab.
The patient was seen post-operatively at week one and informed of the results. He reported no active complaints. Examination showed visual acuity of 20/20 OD and 20/25 OS, with round, regular, and reactive pupils and no afferent pupillary defect. Extraocular movement examination revealed limitations in supraduction. The examination external part of the eye showed that the swelling in the left upper and lower lids had gotten better, while the bleeding and congestion in the conjunctiva had gotten worse. Some stitches were taken out.
The patient was referred to the oncology center in Dammam for confirmation of the diagnosis and to initiate appropriate management based on the disease stage. Magnetic resonance imaging post-surgical resection revealed a left orbital superiorly located a soft tissue extraconal mass lesion inseparable from the superiorly with associated mild mass effect on the adjacent structures as described consistent with the patient’s history of rhambdomyosarcoma. Where he was planned to undergo further adjuvant treatment of chemotherapy.
During the last visit at post-operative week three, the patient reported no active complaints. Examination showed visual acuity of 20/20 OD and 20/32 OS, with persistent limitations in supraduction. The patient was able to slightly open his eye. The anterior segment examination revealed the eyelid appeared normal despite the presence of a suture scar on the left side. All other findings were within normal limits (Figure 7).
Discussion
We report an unusual case of rhabdomyosarcoma (RMS) in childhood, which usually occurs in children, with an average age of 5–7 years [2]. However, our patient was 14 years old. Rhabdomyosarcoma is a highly aggressive tumor and rapidly enlarges [1]. However, our patient had a slower progression, with swelling noticed six weeks previously, which was increasing in size, and non-axial proptosis, being its most common complaint [7]. The supranasal quadrant is the most favorable for RMS in general, but its alveolar subtype arises off the floor [17]. Our patient presented with a supranasal quadrant-based alveolar subtype rhabdomyosarcoma, which extended from the trochlea to the orbital apex. Rhabdomyosarcoma shows different features on X-rays depending on its size, where it is, and how far it has spread. These lesions usually look well defined, uniform, and moderately enhanced on CT scans. Calcifications may be present, particularly in cases of bone erosions. When you look at an MRI, RMS usually looks the same as muscle tissue on T1-weighted imaging (T1WI) and brighter than muscle tissue on T2-weighted imaging (T2WI) [18]. The mass in our patient looked mostly hypointense on T1WI and hyperintense on T2WI, and it had a lot of empty spaces in it. Histologically, RMS can be categorized into three principal subtypes: pleomorphic, alveolar, and embryonal [19]. The embryonal subtype is the most common, and the pleomorphic subtype is the most different and has the best outlook. Conversely, the alveolar subtype, particularly with FOXO1 gene rearrangement, has the worst prognosis [6],[7],[8] [9].[10]. The subtype of our patient was alveolar, as determined by histology. Fluorescence in situ hybridization (FISH) studies on paraffin tissue sections using the FOXO1 gene revealed a negative gene rearrangement in 63.5% of the cells. In comparison, only one FOXO1 copy was present in 25.5% of the cells counted. The absence of FOXO1 rearrangement is clinically significant, as fusion-negative alveolar rhabdomyosarcoma appears to have a relatively better prognosis than fusion-positive disease.
There is no consensus regarding the best method of treatment for RMS. Patients are grouped according to the Intergroup Rhabdomyosarcoma Study Group (IRS) staging scheme (Groups 1 to 4) based on the stage of their disease: Group 1 = completely resected localized tumor, Group 2 = microscopic residual following ex/incisional biopsy, Group 3 = grossly predominant residual (>50% remaining after incisional/excisional biopsy), Group 4 = metastasis [16]. Our patient was entirely debulked and fell in Group 3 according to the IRS staging system. For additional chemotherapy and radiation treatment, he was transferred to a third-level cancer center. Even though orbital RMS rarely spreads, if left untreated, it can spread through hematogenous pathways to the lungs, bone marrow, and bone [1],[6].
According to a study by Zhang et al., surgical resection is associated with a significantly better prognosis, with a 5.7-fold longer survival time [20]. Only 13 of the 144 patients with RMS diagnosed in a study by Markiz et al., which ran from 2005 to 2018, had primary orbital RMS. After five years, the overall survival rate was 64.3%; however, ten years later, it fell to 46.6%. This study emphasizes the prognostic variability and the significance of a timely and accurate diagnosis for improved outcomes [21]. However, if the lesion spreads outside of the eye, especially if it affects the base of the skull, the prognosis deteriorates [22]. Finally, orbital RMS is not common in Saudi Arabia. In a large-scale study by Alkattan et al. investigating the demographics of pediatric orbital lesions, only 11 of 107 studied cases were diagnosed as orbital RMS [23].
Conclusion
In conclusion, a case of orbital alveolar RMS occurring in 14-year-old Saudi boy, from the Eastern Province of Saudi Arabia, is described. Our patient presented atypically as an older child with a prolonged duration of a 6-week history of progressive enlargement and non-axial proptosis, as opposed to common aggressive expansion in early childhood. The atypical presentation of alveolar RMS in the supranasal quadrant with orbital apex involvement illustrates the breadth of clinical presentations and the need for appropriate diagnostic work-up. Radiologic and histopathologic testing were instrumental in the accurate diagnosis of the subtype and disease extent. A multimodal treatment concept (surgical resection, chemotherapy, and irradiation therapy) is emphasized in this scare to avoid an unfavorable prognosis. The findings of this case also contribute to the scarce literature of orbital RMS in our locality and raise awareness to the diversity in prognosis and the necessity of early and accurate diagnosis to optimize outcome. Thus, this case report aims to contribute to the current literature and document an uncommon presentation of orbital RMS. Furthermore, to date, no case report in the literature from the Arabic Gulf region has highlighted the uniqueness and clinical significance of our report. By documenting this rare case, we can enhance the local literature, which may have an impact on clinicians managing cases with a similar presentation in the future. More studies and reports must be pursued to optimize the management and knowledge of this rare pediatric neoplasm.
REFERENCES
1.
Jurdy L, Merks JHM, Pieters BR, Mourits MP, Kloos RJHM, Strackee SD, Saeed P. Orbital rhabdomyosarcomas: A review. Saudi J Ophthalmol 2013;27(3):167–75. [CrossRef]
[Pubmed]

2.
3.
Pontes FSC, de Oliveira JI, de Souza LL, de Almeida OP, Fregnani ER, Vilela RS, et al. Clinicopathological analysis of head and neck rhabdomyosarcoma: A series of 10 cases and literature review. Med Oral Patol Oral Cir Bucal 2018;23(2):e188–97. [CrossRef]
[Pubmed]

4.
Lee RJ, Lee KK, Lin T, Arshi A, Lee SA, Christensen RE. Rhabdomyosarcoma of the head and neck: Impact of demographic and clinicopathologic factors on survival. Oral Surg Oral Med Oral Pathol Oral Radiol 2017;124(3):271–9. [CrossRef]
[Pubmed]

5.
6.
Nhung TH, Minh VL, Tuyet TT, Cuong TM, Lam NL, Trang HT, et al. Orbital rhabdomyosarcoma in a 19-year-old male patient: A case report and literature review. Radiol Case Rep 2023;18(8):2744–9. [CrossRef]
[Pubmed]

7.
Bastola P, Khatiwada S, Khadka M, Dahal P, Bastola S. Diabetic retinopathy among diabetic patients at a tertiary care hospital: A descriptive cross-sectional study. JNMA J Nepal Med Assoc 2022;60(247):234–40. [CrossRef]
[Pubmed]

8.
Parham DM, Alaggio R, Coffin CM. Myogenic tumors in children and adolescents. Pediatr Dev Pathol 2012;15(1 Suppl):211–38. [CrossRef]
[Pubmed]

10.
11.
Topilow NJ, Tran AQ, Koo EB, Alabiad CR. Etiologies of proptosis: A review. Intern Med Rev (Wash DC) 2020;6(3):10.18103/imr.v6i3.852. [CrossRef]
[Pubmed]

12.
Thien HH, Kim Hoa NT, Duy PC, Carlos RG, Son NH. Pediatric primaryorbital rhabdomyosarcoma. Journal of Pediatric Surgery Case Reports 2020;59:101475. [CrossRef]

13.
Ahmad TY, Al Houri HN, Al Houri AN, Ahmad NY. Aggressive orbital rhabdomyosarcoma in adulthood: A case report in a public hospital in Damascus, Syria. Avicenna J Med 2018;8(3):110–3. [CrossRef]
[Pubmed]

14.
Shields CL, Shields JA, Honavar SG, Demirci H. Clinical spectrum of primary ophthalmic rhabdomyosarcoma. Ophthalmology 2001;108(12):2284–92. [CrossRef]
[Pubmed]

15.
Blank LECM, Koedooder K, van der Grient HNB, Wolffs NAW, van de Kar M, Merks JHM, et al. Brachytherapy as part of the multidisciplinary treatment of childhood rhabdomyosarcomas of the orbit. Int J Radiat Oncol Biol Phys 2010;77(5):1463–9. [CrossRef]
[Pubmed]

16.
Shields JA, Shields CL. Rhabdomyosarcoma: Review for the ophthalmologist. Surv Ophthalmol 2003;48(1):39–57. [CrossRef]
[Pubmed]

17.
Karcioglu ZA, Hadjistilianou D, Rozans M, DeFrancesco S. Orbital rhabdomyosarcoma. Cancer Control 2004;11(5):328–33. [CrossRef]
[Pubmed]

18.
Rao AA, Naheedy JH, Chen JYY, Robbins SL, Ramkumar HL. A clinical update and radiologic review of pediatric orbital and ocular tumors. J Oncol 2013;2013:975908. [CrossRef]
[Pubmed]

19.
Parham DM, Barr FG. Classification of rhabdomyosarcoma and its molecular basis. Adv Anat Pathol 2013;20(6):387–97. [CrossRef]
[Pubmed]

20.
Zhang Y, He C, Lian Y, Xiao H. Score for the survival probability of patients with orbital rhabdomyosarcoma after surgery: A long-term and large cohort study. Front Oncol 2020;10:1590. [CrossRef]
[Pubmed]

21.
22.
Das JK, Tiwary BK, Paul SB, Bhattacharjee H, Cida B, Das D. Primary orbital rhabdomyosarcoma with skeletal muscle metastasis. Oman J Ophthalmol 2010;3(2):91–3. [CrossRef]
[Pubmed]

23.
Alkatan HM, Al Marek F, Elkhamary S. Demographics of pediatric orbital lesions: A tertiary eye center experience in Saudi Arabia. J Epidemiol Glob Health 2019;9(1):3–10. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Raghad Mohammad Alakel - Conception of the work, Design of the work, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Saad Algarni - Conception of the work, Design of the work, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Ahd Alharbi - Conception of the work, Design of the work, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Abdulrahman Alhadlag - Conception of the work, Design of the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Hala Nassim - Conception of the work, Design of the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2025 Raghad Alakel et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.