|
Case Series
Unilateral retinal hemorrhages in shaken baby syndrome
1 Michigan State University College of Human Medicine, Grand Rapids, MI, USA
2 Helen Devos Children’s Hospital Grand Rapids, MI, USA
Address correspondence to:
Omi Pang
Michigan State University,
USA
Message to Corresponding Author
Article ID: 100045Z17OP2025
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Pang O, Conley JA. Unilateral retinal hemorrhages in shaken baby syndrome. J Case Rep Images Opthalmol 2025;8(1):1–4.ABSTRACT
Introduction: Bilateral retinal hemorrhages are pathognomonic finding in shaken baby syndrome. The presumed cause of this retinal hemorrhages in the setting of shaken baby syndrome is a repeated acceleration-deceleration injury. However, given the mechanism of injury, bilateral rather than unilateral retinal hemorrhages are expected.
Case Series: We present a series of seven diagnosed cases of shaken baby syndrome in which retinal hemorrhages were unilateral.
Conclusion: Our findings along with existing evidence suggest that the presence of unilateral retinal hemorrhage should not rule out the possibility of child abuse. A comprehensive clinical assessment, including physical examination, imaging, laboratory tests, and history, remains crucial in identifying non-accidental trauma (NAT).
Keywords: Abusive head trauma, Non-accidental trauma, Retinal hemorrhage, Shaken baby syndrome
Introduction
Bilateral retinal hemorrhages are a classic ophthalmologic finding in shaken baby syndrome. In 6% of these cases, an ophthalmologist is the first provider to recognize the abuse [1]. In addition to bilateral retinal hemorrhages, shaken baby syndrome often presents with rib fractures and subdural hematomas, as well as non-specific neurologic symptoms such as seizures or lethargy [2].
A systematic review of retinal hemorrhages in abusive vs non-abusive head trauma showed that in a child presenting with retinal hemorrhage, the probability of abuse is 91% [3]. Repetitive acceleration-deceleration is a putative mechanism by which these retinal injuries occur in the setting of shaken baby syndrome, which would imply that both eyes should be involved [2]. Yet in another systematic review of abusive vs non-abusive head trauma, approximately 17% of retinal hemorrhages were unilateral in abusive head trauma [3]
Although retinal hemorrhages are unlikely to be found in non-abusive head trauma, when present, they are more likely to be unilateral [3]. Other potential etiologies of retinal hemorrhage in children, though rare, include coagulopathies [4]. Other trauma-related injuries can result in retinal hemorrhages. However, these require significant force and include fatal car accidents and falls over 10 meters [3].
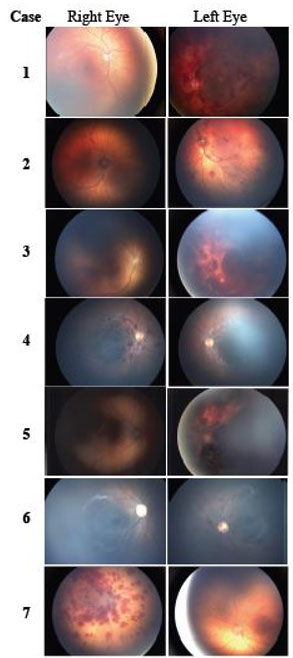
Here we present a series of 7 diagnosed cases of shaken baby syndrome in which retinal hemorrhages were observed to be unilateral. Retinal photos for each case are included to demonstrate the variety of presentations observed in unilateral retinal hemorrhage. We aim to contribute to the growing body of reports describing the presence of unilateral retinal hemorrhage in the setting of shaken baby syndrome with the hope of ensuring that non-accidental trauma is included in the differential of unilateral retinal hemorrhages.
Case Series
Case 1
An 8-month-old female with a history of prematurity, torticollis, and plagiocephaly presented to the emergency department with seizures and unresponsiveness. Non-contrast head computed tomography (CT) showed bilateral subdural hemorrhages on the left greater than right and an anoxic brain. Examination showed periorbital edema.
Indirect ophthalmoscopy showed left macular schisis and multiple diffuse intraretinal hemorrhages and a normal right eye exam (Figure 1, Case 1). The patient developed refractory intracranial hypertension and progressed to brain death. On further inquiry the history of shaking the baby was elicited.
Case 2
A previously healthy 2-month-old male was admitted for altered mental status. Physical examination revealed a full fontanelle and periorbital ecchymosis of the right eye. Non-contrast head CT showed multifocal bilateral small subdural hematomas, bilateral frontal and parietal surface hemorrhagic contusions, and non-occlusive thrombosis of the superior sagittal sinus. Skeletal survey exhibited bilateral rib fractures.
Indirect ophthalmoscopy demonstrated approximately 20 intraretinal hemorrhages in the posterior pole to mid-periphery of the left eye (Figure 1, Case 2). There was one chorioretinal scar in the right eye, but no retinal hemorrhage. On further inquiry the history of shaking the baby was elicited.
Case 3
A 2-month-old male with a history of prematurity and twin gestation presented to the emergency department with status epilepticus. Non-contrast head CT showed bilateral acute supra- and infratentorial subdural hematomas. A skeletal survey indicated healing right-sided rib and bilateral tibial fractures.
Indirect ophthalmoscopy revealed multilayered retinal hemorrhages in all four quadrants of the left eye (Figure 1, Case 3). On further inquiry the history of shaking the baby was elicited.
Case 4
A previously healthy 6-month-old female with a history of torticollis presented to the emergency department with fatigue and vomiting. On physical exam, there was a chest abrasion and ecchymosis over the right shoulder. Non-contrast head CT showed subdural hematomas. Skeletal survey was unremarkable.
Indirect ophthalmoscopy of the retina showed multiple intraretinal and a few small preretinal hemorrhages in the posterior pole of the right eye (Figure 1, Case 4). She was diagnosed with NAT and placed in foster care.
Case 5
A previously healthy 2-month-old male presented to the emergency department for lethargy and decreased oral intake. On exam, there was bruising to the chest and abdomen. Magnetic resonance imaging (MRI) of the brain revealed bilateral subdural hemorrhages and a subarachnoid hemorrhage. Skeletal survey was unremarkable.
Indirect ophthalmoscopy showed left retinal hemorrhages in multiple layers, extending to the ora serrata (Figure 1, Case 5). On further inquiry the history of shaking the baby was elicited.
Case 6
A previously healthy 7-month-old male presented to the emergency department after a reported 3-feet fall onto carpeted floor. The patient was unresponsive with a fixed, dilated pupil and decerebrate posturing of the bilateral upper extremities. Non-contrast head CT showed a large left extra-axial hemorrhage. Skeletal survey was unremarkable.
Indirect ophthalmoscopy demonstrated scattered intra- and pre-retinal hemorrhages of the left eye (Figure 1, Case 6). On further inquiry the history of shaking the baby was elicited.
Case 7
A 2-month-old female with a history of humeral fracture and perineal lesion presented to the emergency department with altered mental status and respiratory failure. The patient had no spontaneous movement. There was bruising over the left eye, nose, and ear with a scab of the right nares. Non-contrast head CT revealed subdural hemorrhage and bilateral skull fractures. Bone survey showed healing rib fractures.
Indirect ophthalmoscopy revealed retinal hemorrhages of the right eye, which were too numerous to count in multiple layers, extending to the ora serrata (Figure 1, Case 7). On further inquiry the history of shaking the baby was elicited.
Discussion
This report contributes to the growing body of literature that suggests that while uncommon in the setting of shaken baby syndrome, unilateral retinal hemorrhages should not be used to dismiss the possibility of abuse. In all other reported cases of unilateral retinal hemorrhages associated with NAT, there were other objective findings to suggest abuse (e.g., positive findings on head CT, skeletal studies, radiography) [5],[6],[7],[8]. This is consistent with the cases in the present report. However, in very rare cases, retinal hemorrhages may occur without or prior to objective findings such as intracranial bleeding on imaging [9],[10].
While the primary mechanism of unilateral retinal hemorrhage remains unclear, several causes have been proposed. In their report, Drack et al. suggest that a strong hand preference of the abuser may be an important mechanism of unilateral retinal hemorrhages. A strong hand preference in the abuser may cause rotational acceleration along the axial plane in addition to the rostral-caudal axis, leading to hemorrhage of one and not both retinas. Strong hand preference may cause twisting of the neck and increase unilateral jugular occlusion, disproportionately increasing the intracranial pressure on one side greater than another [5]. In our case series, 5 out of 7 cases had left retinal hemorrhages. Given the prevalence of right-handedness in the general population, it is possible that this may be a major contributing factor. However, there is no data on the handedness of the assailants. Another possible reason for finding unilateral retinal hemorrhages on exam in NAT cases may be delayed presentation of shaken baby syndrome in which interval healing has occurred. This was not likely in the cases presented in this case series as these patients presented to the emergency department within 24 hours of initial symptom onset.
Conclusion
Accurately identifying child abuse is difficult, yet urgently important. In <50% of NAT cases, suspected abusers confess to the physical abuse. The finding of unilateral retinal hemorrhages should not be used to rule out NAT. Instead, clinical correlation with physical examination, skeletal survey, head CT, labs, and history play crucial roles in making an accurate diagnosis.
REFERENCES
1.
American Academy of Ophthalmology [Internet]. 2015. Abusive Head Trauma/Shaken Baby Syndrome - 2015. [Available at: https://www.aao.org/education/clinical-statement/abusive-head-traumashaken-baby-syndrome]

2.
Mian M, Shah J, Dalpiaz A, et al. Shaken baby syndrome: A review. Fetal Pediatr Pathol 2015;34(3):169–75. [CrossRef]
[Pubmed]

3.
Maguire SA, Watts PO, Shaw AD, et al. Retinal haemorrhages and related findings in abusive and non-abusive head trauma: A systematic review. Eye (Lond) 2013;27(1):28–36. [CrossRef]
[Pubmed]

4.
Thau A, Saffren B, Anderst JD, Carpenter SL, Levin AV. A review on clotting disorders and retinal hemorrhages: Can they mimic abuse? Child Abuse Negl 2021;118:105070. [CrossRef]
[Pubmed]

5.
Drack AV, Petronio J, Capone A. Unilateral retinal hemorrhages in documented cases of child abuse. Am J Ophthalmol 1999;128(3):340–4. [CrossRef]
[Pubmed]

6.
Paviglianiti JC, Donahue SP. Unilateral retinal hemorrhages and ipsilateral intracranial bleeds in nonaccidental trauma. J AAPOS 1999;3(6):383–4. [CrossRef]
[Pubmed]

7.
Tyagi AK, Willshaw HE, Ainsworth JR. Unilateral retinal haemorrhages in non-accidental injury. Lancet 1997;349(9060):1224. [CrossRef]
[Pubmed]

8.
Arlotti SA, Forbes BJ, Dias MS, Bonsall DJ. Unilateral retinal hemorrhages in shaken baby syndrome. J AAPOS 2007;11(2):175–8. [CrossRef]
[Pubmed]

9.
Burkhart ZN, Thurber CJ, Chuang AZ, Kumar KS, Davis GH, Kellaway J. Risk factors associated with retinal hemorrhage in suspected abusive head trauma. J AAPOS 2015;19(2):119–23. [CrossRef]
[Pubmed]

10.
Jenny C, Hymel KP, Ritzen A, Reinert SE, Hay TC. Analysis of missed cases of abusive head trauma. JAMA 1999;281(7):621–6. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Omi Pang - Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Julie A Conley - Conception of the work, Design of the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2025 Omi Pang et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.