|
Case Report
Focal laser and intravitreal bevacizumab for choroidal neovascularization secondary to Grönblad–Strandberg syndrome
1 FRCSEd, FWACS, DRCOphth, MSc, Clinical Research Consultant Ophthalmologist, Retinal Unit, Eye Foundation Hospital, 27 Issac John Street, Ikeja GRA, Lagos, Nigeria
2 FWACS, FMCOph, Consultant Ophthalmologist, Retinal Unit, Eye Foundation Hospital, 27 Issac John Street, Ikeja GRA, Lagos, Nigeria
Address correspondence to:
Toyin Akanbi
Retinal Unit, Eye Foundation Hospital, 27 Isaac John Street, Ikeja GRA, Lagos,
Nigeria
Message to Corresponding Author
Article ID: 100036Z17OO2023
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Oderinlo O, Akanbi T. Focal laser and intravitreal bevacizumab for choroidal neovascularization secondary to Grönblad–Strandberg syndrome. J Case Rep Images Opthalmol 2023;6(1):5–8.ABSTRACT
Introduction: Pseudoxanthoma elasticum is a rare genetic disorder. It has several ocular features including angioid streaks and choroidal neovascularization which can significantly affect vision.
Case Report: A 50-year-old man presented with nine months history of poor vision affecting both distant and near vision. His best corrected visual acuities were 6/18 right eye and 1/60 left eye. His anterior segments were normal. Funduscopy revealed linear hyperpigmented irregular branching peripapillary lesions; angioid streaks both eyes. He had bilateral speckled retina pigment epithelial hyperpigmented lesions interspaced with dot hemorrhages in the macula region suggestive of likely choroidal neovascularization. He had “peau d’orange” skin appearance around his neck. Fundus fluorescein angiography showed features of occult subfoveal choroidal neovascularization. He was referred to a physician and had a skin biopsy which revealed histologic features of Pseudoxanthoma elasticum. He was treated with bilateral focal argon laser. However he had right intravitreal Bevacizumab after a large ipsilateral subfoveal hemorrhage. His visual acuities remained stable afterward.
Conclusion: Patients with Pseudoxanthoma elasticum have to be closely monitored for ocular manifestations. Choroidal neovascularization should be detected early and promptly treated. Antivascular endothelial growth factor injections have become the preferred treatment option for choroidal neovascularization in these patients.
Keywords: Bevacizumab, Choroidal neovascularization, Laser, Pseudoxanthoma elasticum
Introduction
Pseudoxanthoma elasticum (PXE) is a genetic metabolic disease with autosomal recessive inheritance caused by mutations in the ABCC6 gene [1]. It affects the skin, eyes, and cardiovascular system, there is progressive calcification and fragmentation of elastic fibers in the affected tissues [2].
The association between retinal angioid streaks and skin features in PXE was reported by Grönblad and by Strandberg in 1929 [3],[4] and PXE is referred to as Grönblad–Strandberg syndrome.
Ocular features of PXE include angioid streaks, peau d’orange, comet lesions, choroidal neovascularization (CNV), chorioretinal atrophy, subretinal fluid independent from CNV, pattern dystrophy-like changes, debris accumulation under the retinal pigment epithelium, and reticular drusen [5]. Angioid streaks are the most obvious and most observed funduscopic finding in these patients [5]. Choroidal neovascularization is a frequent complication in patients with PXE and it may cause pronounced vision loss [5].
Case Report
A 50-year-old Nigerian man presented with nine months history of poor vision affecting both distant and near vision. He complained of seeing flashes of light in the right eye. He had worn corrective spectacles for 10 years. His mother had been treated for glaucoma, his father also had poor vision, the cause was not known.
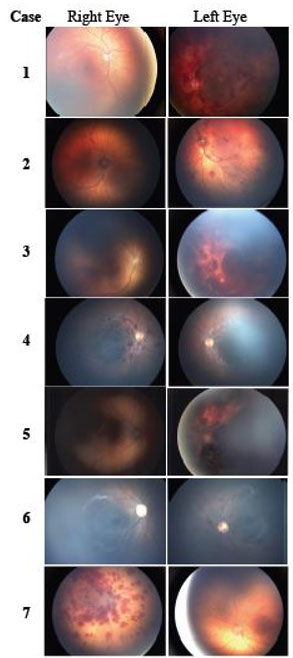
Ocular examination revealed best corrected visual acuities 6/18 right eye (OD) and 1/60 left eye (OS). His anterior segments were normal bilaterally (OU). Intraocular pressures were 10 mmHg OU; he had early lens opacities OU. Funduscopy revealed linear hyperpigmented irregular branching peripapillary lesions (angioid streaks) OU. He also had speckled retina pigment epithelial hyperpigmented lesions interspaced with dot hemorrhages in the macula region suggestive of choroidal neovascularization OU (Figure 1). Fundus fluorescein angiography (FFA) showed bilateral peripapillary hyperfluorescent branching patterns as a result of unmasking of choroidal fluorescence and stippled non-homogenous hyperfluorescent macular pattern with irregular edges suggestive of occult subfoveal choroidal neovascularization (Figure 2). He had “peau d’orange” skin appearance around the neck (Figure 3). His cardiovascular system was normal.
He was referred to a physician, his cardiovascular system was normal but his skin biopsy revealed swollen and irregularly clumped altered elastin fibers within the middle and lower thirds of the dermis with mild basophilic staining. There were also foci of accumulation of basophilic acellular materials within the vicinity of the elastin fibers with mild chronic inflammatory cellular infiltrates. He was diagnosed with Grönblad–Strandberg syndrome.
He was treated with bilateral focal argon laser (250 µm × 0.12 mW × 122 pulses). Five months later he developed a large subfoveal hemorrhage OD and a disciform scar OS. His visual acuity had reduced to hand movement OD and 6/36 in OS. He had one dose of intravitreal Bevacizumab 1.25 ug/0.05 mg OD and more laser photocoagulation OD three months later with complete resolution of choroidal neovascularization and stabilization of visual acuity.
Discussion
There is no cure for PXE and patients should be monitored on a regular basis [1]. The most severe ocular complication of PXE is CNV [6]. Untreated CNV results in subretinal bleeding and exudation, leading to fibrovascular scarring and a progressive loss of vision [5].
Our patient had bilateral CNV; he was treated with bilateral focal laser and intravitreal Bevacizumab OD with stabilization of his visual acuity. Bevacizumab was given OD post focal laser when he developed a huge subfoveal hemorrhage.
Gliem et al. reported that laser photocoagulation yielded comparable results as photodynamic therapy; however, the application of laser was mostly restricted to extrafoveal lesions; it was complicated by frequent recurrences, and led to more retinal damage with subsequent absolute scotomas [7].
The use of intravitreal anti-vascular endothelial growth factors (VEGF) have been documented in several case reports, case series, and clinical trials and they have become the first-choice treatment for CNV secondary to angioid streaks and the ocular manifestations of PXE [8].
Intravitreal Bevacizumab [9],[10],[11], Ranibizumab [12], Aflibercept [13], and Conbercept [14] have been used in treating CNV associated with PXE.
Finger et al. reported that intravitreal Bevacizumab therapy demonstrates long-term effectiveness by preserving function in advanced disease and improving function in early disease [11].
Conclusion
Pseudoxanthoma elasticum is a rare disease. Patients with PXE have to be closely monitored for ocular manifestations. It may be associated with CNV which can cause significant visual impairment. Choroidal neovascularization should be detected early and promptly treated. Intravitreal anti-VEGF injections have become the mainstay of treatment for CNV in these patients.
REFERENCES
1.
Germain DP. Pseudoxanthoma elasticum. Orphanet J Rare Dis 2017;12(1):85. [CrossRef]
[Pubmed]

2.
Finger RP, Charbel Issa P, Ladewig MS, et al. Pseudoxanthoma elasticum: Genetics, clinical manifestations and therapeutic approaches. Surv Ophthalmol 2009;54(2):272–85. [CrossRef]
[Pubmed]

5.
Gliem M, Zaeytijd JD, Finger RP, Holz FG, Leroy BP, Charbel Issa P. An update on the ocular phenotype in patients with pseudoxanthoma elasticum. Front Genet 2013;4:14. [CrossRef]
[Pubmed]

6.
Georgalas I, Papaconstantinou D, Koutsandrea C, et al. Angioid streaks, clinical course, complications, and current therapeutic management. Ther Clin Risk Manag 2009;5(1):81–9.
[Pubmed]

7.
Gliem M, Finger RP, Fimmers R, Brinkmann CK, Holz FG, Charbel Issa P. Treatment of choroidal neovascularization due to angioid streaks: A comprehensive review. Retina 2013;33(7):1300–14. [CrossRef]
[Pubmed]

8.
Stumpf MJ, Schahab N, Nickenig G, Skowasch D, Schaefer CA. Therapy of pseudoxanthoma elasticum: Current knowledge and future perspectives. Biomedicines 2021;9(12):1895. [CrossRef]
[Pubmed]

9.
Cărăuş CV, Spînu AM, Negrii AA. Case report: Grönblad-Strandberg syndrome. Rom J Ophthalmol 2022;66(2):158–63. [CrossRef]
[Pubmed]

10.
Kyo A, Yamamoto M, Honda S. A case of angioid streaks that produced choroidal neovascularization after the onset of unilateral acute retinopathy in pseudoxanthoma elasticum. Am J Ophthalmol Case Rep 2022;27:101591. [CrossRef]
[Pubmed]

11.
Finger RP, Charbel Issa P, Schmitz-Valckenberg S, Holz FG, Scholl HN. Long-term effectiveness of intravitreal bevacizumab for choroidal neovascularization secondary to angioid streaks in pseudoxanthoma elasticum. Retina 2011;31(7):1268–78. [CrossRef]
[Pubmed]

12.
Mimoun G, Ebran JM, Grenet T, Donati A, Cohen SY, Ponthieux A. Ranibizumab for choroidal neovascularization secondary to pseudoxanthoma elasticum: 4-year results from the PIXEL study in France. Graefes Arch Clin Exp Ophthalmol 2017;255(8):1651–60. [CrossRef]
[Pubmed]

13.
Gliem M, Birtel J, Herrmann P, et al. Aflibercept for choroidal neovascularizations secondary to pseudoxanthoma elasticum: A prospective study. Graefes Arch Clin Exp Ophthalmol 2020;258(2):311–8. [CrossRef]
[Pubmed]

14.
Cui C, Zhou Z, Zhang Y, Sun D. A case report: Pseudoxanthoma elasticum diagnosed based on ocular angioid streaks and the curative effect of Conbercept treatment. BMC Ophthalmol 2021;21(1):307. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Olufemi Oderinlo - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Toyin Akanbi - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2023 Olufemi Oderinlo et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.