|
Case Report
0.19 mg Fluocinolone acetonide implant (ILUVIEN) in the treatment of birdshot chorioretinopathy: A case report
1 Department of Ophthalmology, University Hospital Galway, Galway City, Co. Galway, Ireland
Address correspondence to:
Shane Whitlow
Department of Ophthalmology, University Hospital Galway, Galway City, Co. Galway,
Ireland
Message to Corresponding Author
Article ID: 100025Z17SW2022
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Whitlow S, O’Dwyer G, Townley D. 0.19 mg Fluocinolone acetonide implant (ILUVIEN) in the treatment of birdshot chorioretinopathy: A case report. J Case Rep Images Opthalmol 2022;5:100025Z17SW2022.ABSTRACT
Introduction: Birdshot choroidopathy (BCR) is a non-infectious posterior uveitis. Long-lasting resolution of BCR associated cystoid macular edema (CME) can be difficult to achieve with current accepted treatments due to its high rate of recurrence. A 0.19 mg fluocinolone acetonide implant (FA; ILUVIEN, Alimera Sciences Ltd., Hampshire, UK) is a slow release, intravitreal, non-biodegradable corticosteroid implant that can be used in the management of recurrent non-infectious uveitis affecting the posterior segment of the eye. We report a case following treatment of recurrent BCR associated CME with the FA implant.
Case Report: This case is from a patient diagnosed with BCR with recurrent CME, which failed to resolve following multiple dexamethasone implant administrations. Following delivery of the FA implant, a sustained improvement in best-corrected visual acuity and central macular thickness was observed.
Conclusion: Based on current data, we recommend consideration of treatment with the FA implant
Keywords: Birdshot choroidopathy, Cystoid macular edema, Fluocinolone acetonide, ILUVIEN, Ozurdex, Uveitis
Introduction
Birdshot chorioretinopathy (BCR) is a rare condition (0.6–1.5% of uveitis referred to tertiary centers) that is well described in the literature yet a poorly understood cause of posterior uveitis [1]. Birdshot chorioretinopathy is a chronic inflammatory condition [1],[2] typically occurring in females in their later 40–50s where immunosuppression is required to reduce the progression of disease [1],[3].
The 0.19 mg fluocinolone acetonide implant (FA; ILUVIEN, Alimera Sciences, Hampshire, UK) is a slow release (0.2 mcg/day), intravitreal, non-biodegradable corticosteroid implant that lasts for up to three years. In 2019, the FA implant was approved in Europe for the prevention of relapse in recurrent non-infectious uveitis affecting the posterior segment of the eye. In the United States, a 0.59 mg fluocinolone acetonide intravitreal implant (Retisert; Bausch Health Ireland Limited, Ireland) [4] is indicated for the treatment of chronic non-infectious uveitis affecting the posterior segment of the eye. This implant is surgically implanted into the posterior segment of the affected eye through a pars plana incision and releases between 0.3 and 0.4 mcg/day over approximately 30 months. However, this treatment is not licensed for use in Europe [4].Another intravitreal corticosteroid implant approved in Europe for use in posterior segment non-infectious uveitis is the dexamethasone implant (Ozurdex; Allergan Pharmaceuticals Ireland, Westport, Ireland) [5].
Recent studies have shown a decrease in the reoccurrence of posterior uveitis following treatment with the FA implant [6],[7]. Indeed, the study by Jaffe et al. [4], reporting 12-month outcomes in a study designed to last 36 months, concluded that the FA implant provided effective management of intraocular inflammation associated with non-infectious posterior uveitis as shown by lower recurrence rates, fewer uveitis recurrences per study eye and a longer time to onset of recurrence compared to sham injection. The duration of action of the FA implant is still being studied in real-world practices, but the study by Meira et al. [7] reported sustained control of inflammation for up to three years after therapy with the FA implant with improvements in best-corrected visual acuity (BCVA) and central macular thickness (CMT).
A review of the literature reveals that the FA (Retisert) has been previously implanted to control inflammation in BCR [8].
Case Report
We report the case of a 55-year-old woman who was referred to our clinic with a diagnosis of intermediate uveitis in August 2016.
The patient was seen by an ophthalmologist three years ago. Then she complained of a decrease in vision in her right eye and on examination had vitritis and vasculitis. The patient was given a course of oral steroids and the patient symptoms improved.
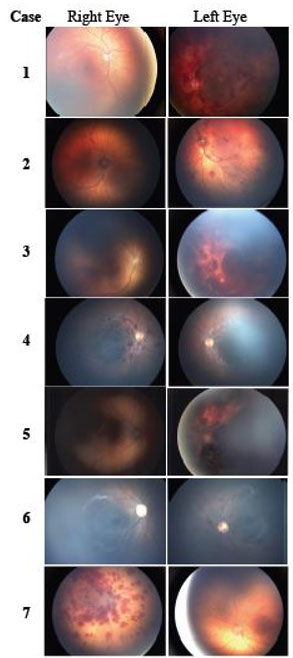
On initial presentation to our clinic the patient had a visual acuity (VA) of 6/15 in the right eye and 6/6 in the left eye. The patient had a normal anterior segment. Dilated fundal exam demonstrated bilateral 2+ vitreous cells. The retinal clinical findings are shown in Figure 1 and together supported a diagnosis of BCR in the right eye. The patient was started on 60 mg of steroid and treated with dexamethasone implant after the tuberculosis tests came back negative. The patient’s vision improved to 6/9 in the right eye following treatment with the dexamethasone implant.
Serology work-up included full blood count, urea, and electrolytes and liver function tests, which were all within normal ranges. Venereal disease research laboratory (VDRL), antinuclear antibody, antineutrophil cytoplasmic antibody (ANCA) levels, Mantoux and QuantiFERON tests were all negative. A chest X-ray was reported as normal. An magnetic resonance imaging (MRI) brain showed no evidence of demyelination or space occupying lesion. Haplotyping showed a positive HLA-A29 result while HLA-B27 was negative.
The patient was started on 750 mg BD of Mycophenolate mofetil (MMF) in order to reduce ocular inflammation and in turn oral steroids were tapered. Four months following dexamethasone implant administration, the patient’s vision decreased further to 6/12. Figure 2 represents a graph of CMT and BCVA and shows a correlation between improvements in CMT and BCVA.
Mycophenolate mofetil was increased and a second dexamethasone implant was administered to the patient. Four months later, the patient’s VA decreased to 6/15 with a concomitant return of CME, due to the recurrent CME a total of five intravitreal dexamethasone implant was given to the patient.
Throughout the course of treatment with dexamethasone implant the patient slowly developed a posterior subcapsular cataract. Clinically this became more evident after the fifth dexamethasone implant was administered, resulting in a marked reduction in BCVA. Therefore, the patient underwent elective uncomplicated cataract surgery.
Given the numerous recurrences of CME, it was felt that the immunosuppressive treatment should be increased and therefore Adalimumab was started. Unfortunately, once again the CME returned, necessitating a change in therapy that would provide a longer-term therapeutic benefit. The left eye was quiescent on Adalimumab, but the right eye was progressing and therefore an FA implant was given to the patient. The patient’s vision improved to 6/6 and the CME has resolved with no further recurrence or need for additional injections in the 12 months after therapy with the FA implant. Figure 3 demonstrates the improvement in field loss as measured by Humphrey visual field from first presentation to treatment with immunosuppressive therapy and finally immunosuppression and ILUVIEN.
Discussion
Birdshot chorioretinopathy is a chronic inflammatory condition that can potentially be sight threatening. This case describes the sustained management of CME following therapy with an FA implant. This effect was observed after numerous prior therapies (including intravitreal injection of a dexamethasone implant, systemic steroids, and immunosuppressants) and recurrences of CME.
Fluocinolone acetonide has previously been employed to successfully decrease intraocular inflammation [9] but has well-known side effects including raised intraocular pressure and cataract development [9],[10]. The current case is the first to describe the effectiveness of the FA implant following the diagnosis of BCR [1],[11]. The flattening of the macula in Figure 2 demonstrates the effectiveness of the FA implant with reduced recurrences, as seen by the lower variability in the measurements of CMT. Following administration of an FA implant, and subsequent cataract surgery, a higher visual acuity was attained than that at presentation. As there was no evidence of cataract at presentation, we believe that the favorable visual outcome in this case was due to sustained resolution of macular edema achieved with the FA implant.
A review of the literature provides several published examples of treatment of BCR with intravitreal steroids. This case illustrates that the FA implant may be beneficial to patients suffering from decreased VA secondary to BCR associated CME. Additionally, it also shows that due to the FA implant having a much longer release than the dexamethasone implant, it may be useful in patients with recurrent CME as well as reducing the number of recurrences.
Conclusion
Based on the current data, we recommend consideration of treatment with the FA implant in patients with recurrence of CME secondary to BCR. We hope that further published cases or trials will find similar success and provide optimal treatment plans for patients suffering from this rare condition.
REFERENCES
1.
Shah KH, Levinson RD, Yu F, et al. Birdshot chorioretinopathy. Surv Ophthalmol 2005;50(6):519–41. [CrossRef]
[Pubmed]

2.
Gasch AT, Smith JA, Whitcup SM. Birdshot retinochoroidopathy. Br J Ophthalmol 1999;83(2):241–9. [CrossRef]
[Pubmed]

3.
Thorne JE, Jabs DA, Peters GB, Hair D, Dunn JP, Kempen JH. Birdshot retinochoroidopathy: Ocular complications and visual impairment. Am J Ophthalmol 2005;140(1):45–51. [CrossRef]
[Pubmed]

4.
Jaffe GJ, Martin D, Callanan D, et al. Fluocinolone acetonide implant (Retisert) for noninfectious posterior uveitis: Thirty-four-week results of a multicenter randomized clinical study. Ophthalmology 2006;113(6):1020–7. [CrossRef]
[Pubmed]

5.
Lowder C, Belfort R Jr, Lightman S, et al. Dexamethasone intravitreal implant for noninfectious intermediate or posterior uveitis. Arch Ophthalmol 2011;129(5):545–53. [CrossRef]
[Pubmed]

6.
Jaffe GJ, Foster CS, Pavesio CE, Paggiarino DA, Riedel GE. Effect of an injectable fluocinolone acetonide insert on recurrence rates in chronic noninfectious uveitis affecting the posterior segment: Twelve-month results. Ophthalmology 2019;126(4):601–10. [CrossRef]
[Pubmed]

7.
Meira J, Madeira C, Falcão-Reis F, Figueira L. Sustained control from recurring non-infectious uveitic macular edema with 0.19 mg fluocinolone acetonide intravitreal implant – A case report. Ophthalmol Ther 2019;8(4):635–41. [CrossRef]
[Pubmed]

8.
Menezo V, Taylor SR. Birdshot uveitis: Current and emerging treatment options. Clin Ophthalmol 2014;8:73–81. [CrossRef]
[Pubmed]

9.
Rush RB, Goldstein DA, Callanan DG, Meghpara B, Feuer WJ, Davis JL. Outcomes of birdshot chorioretinopathy treated with an intravitreal sustained-release fluocinolone acetonide-containing device. Am J Ophthalmol 2011;151(4):630–6. [CrossRef]
[Pubmed]

10.
Bollinger K, Kim J, Lowder CY, Kaiser PK, Smith SD. Intraocular pressure outcome of patients with fluocinolone acetonide intravitreal implant for noninfectious uveitis. Ophthalmology 2011;118(10):1927–31. [CrossRef]
[Pubmed]

11.
Levinson RD, Brezin A, Rothova A, Accorinti M, Holland GN. Research criteria for the diagnosis of birdshot chorioretinopathy: Results of an international consensus conference. Am J Ophthalmol 2006;141(1):185–7. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Shane Whitlow - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Gareth O’Dwyer - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Deirdre Townley - Conception of the work, Design of the work, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2022 Shane Whitlow et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.