|
Clinical Image
Scleritis in Takayasu’s arteritis
1 MBBS, BSc (Hons), Internal Medicine Resident, Internal Medicine, Tan Tock Seng Hospital, Singapore
2 MBBS, MMed (Ophth), FRCOphth (UK), FAM, Consultant, Ophthalmology, Tan Tock Seng Hospital, Singapore
Address correspondence to:
Gareth Lim
11 Jalan Tan Tock Seng, Singapore 308433,
Singapore
Message to Corresponding Author
Article ID: 100023Z17GL2021
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Lim G, Fang HM. Scleritis in Takayasu’s arteritis. J Case Rep Images Opthalmol 2021;4:100023Z17GL2021.ABSTRACT
No Abstract
Keywords: Scleritis, Takayasu’s arteritis, Vasculitis
Case Report
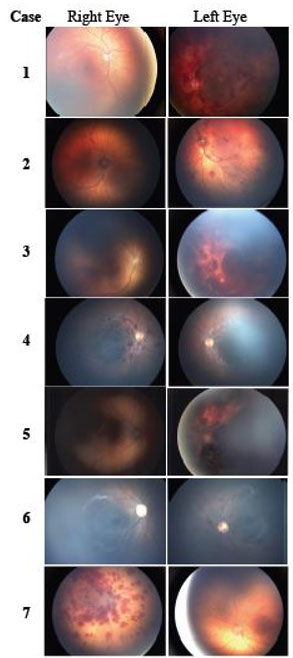
A 52-year-old Indian lady with no past medical history presented with three acute self-limiting episodes of a painful red right eye over the course of a year. There was photophobia but no loss of vision. Closer examination of her eye revealed anterior scleritis and scleromalacia (Figure 1A). She also had worsening dyspnoea, fatigue, and unintentional weight loss over the last few months. There was no history of limb claudication. On examination, peripheral pulses were present throughout but there was a differential brachial blood pressure in her arms. No bruits were auscultated over her carotid, subclavian, interscapular, and abdominal aorta regions. Cardiovascular evaluation revealed severe aortic regurgitation and cardiomyopathy. A computed tomography aortogram showed extensive ascending and descending thoracic aortitis and mediastinal lymphadenopathy, (Figure 1B, arrows) as well as inflammation of the right brachiocephalic and left carotid arteries. Her erythrocyte sedimentation rate was raised at 72 millimeter/hour (0 to 20 millimeter/hour). Anti-nuclear antibodies (ANA), anti-double stranded DNA antibodies (ds-DNA), and antineutrophil cytoplasmic antibodies (ANCA) were negative. Evaluation for tuberculosis and syphilis was negative. Our patient only fulfilled 2 of the 6 American College of Rheumatology (ACR) diagnostic criteria for Takayasu’s arteritis (differential BP and arteriographic narrowing). However, the ACR criteria are mainly used as a research tool and have limited use in clinical practice. Given the constellation of clinical features and extensive large-vessel involvement, a diagnosis of Takayasu’s arteritis was made. She was started on intravenous methylprednisolone and cyclophosphamide with improvement in her symptoms.
Discussion
Takaysu’s arteritis is a large vessel vasculitis with a predilection for the aorta and its major branches. Ocular manifestations of Takayasu’s arteritis have a prevalence of 8.1–68% [1]. They include retinal artery and vein occlusion, hypertensive retinopathy, Takayasu’s retinopathy and treatment-related complications such as steroid-induced glaucoma. However, only a handful of cases in the literature describe an association between scleritis and the disease [2],[3],[4],[5],[6],[7],[8],[9]—a feature more commonly found in small vessel vasculitis. It is important to recognize this association as early treatment can lead to significant improvement in symptoms and better disease control.
Conclusion
Scleritis can be the first manifestation of Takayasu’s arteritis. Clinicians should be aware of this as it is a debilitating disease that can be easily treated.
REFERENCES
1.
Peter J, David S, Danda D, Peter JV, Horo S, Joseph G. Ocular manifestations of Takayasu arteritis: A cross-sectional study. Retina 2011;31(6):1170–8. [CrossRef]
[Pubmed]

2.
Sureja NP, Kalyan S, Patel MR. Recurrent scleritis as a presenting manifestation of asymptomatic occult Takayasu arteritis. Rheumatol Adv Pract 2020;5(1): rkaa065. [CrossRef]
[Pubmed]

3.
Smith JR, Rosenbaum JT. Case reports and small case series: Scleritis occurring in association with Takayasu disease. Arch Ophthalmol 2001;119(5):778–9.
[Pubmed]

4.
Chaudhary M, Shah DN, Chaudhary RP. Scleritis and Takayasu’s disease – rare combined presentation. Nepal J Ophthalmol 2017;9(18):170–4. [CrossRef]
[Pubmed]

5.
Jain R, Ionides A, Pavesio C, Russell A, Haskard D. Scleritis as a presenting feature of Takayasu’s disease. Br J Ophthalmol 2000;84(7):801. [CrossRef]
[Pubmed]

6.
Arya SK, Nahar R, Narang S, Jain R, Kalra N, Sood S. Sclerokeratitis in Takayasu’s arteritis: A case report. Jpn J Ophthalmol 2005;49(6):548–50. [CrossRef]
[Pubmed]

7.
Amer R, Rankin R, Mackenzie J, Olson J. Posterior scleritis: An ominous sign of occult Takayasu’s arteritis. Br J Ophthalmol 2007;91(11):1568–9. [CrossRef]
[Pubmed]

8.
Shukla E, Desai A, Malkan N, Gokhale Y. Nodular scleritis as a presenting feature of Takayasu’s arteritis. Indian J Ophthalmol 2016;64(4):312–4. [CrossRef]
[Pubmed]

9.
Akhtar S, Babar S, Lightman S, Mason JC. Adalimumab-induced remission of anterior scleritis: A very rare late manifestation of Takayasu arteritis. Rheumatology (Oxford) 2015;54(12):2288–90. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Gareth Lim - Conception of the work, Design of the work, Acquisition of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Helen Mi Fang - Conception of the work, Design of the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2021 Gareth Lim et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.